Article co-authored with Sarina Gandhi.
Our collective response to Covid-19 has radically changed the way that we currently live. Smaller class sizes, homeschooling, reduced interactions with peers and family, and heightened sanitization inarguably affect our children mentally, physically, and socially. But in the years following the resolution of the pandemic, what might be the impact of all this extra hygiene on the development of a child’s immune system?
Too-Clean Hygiene
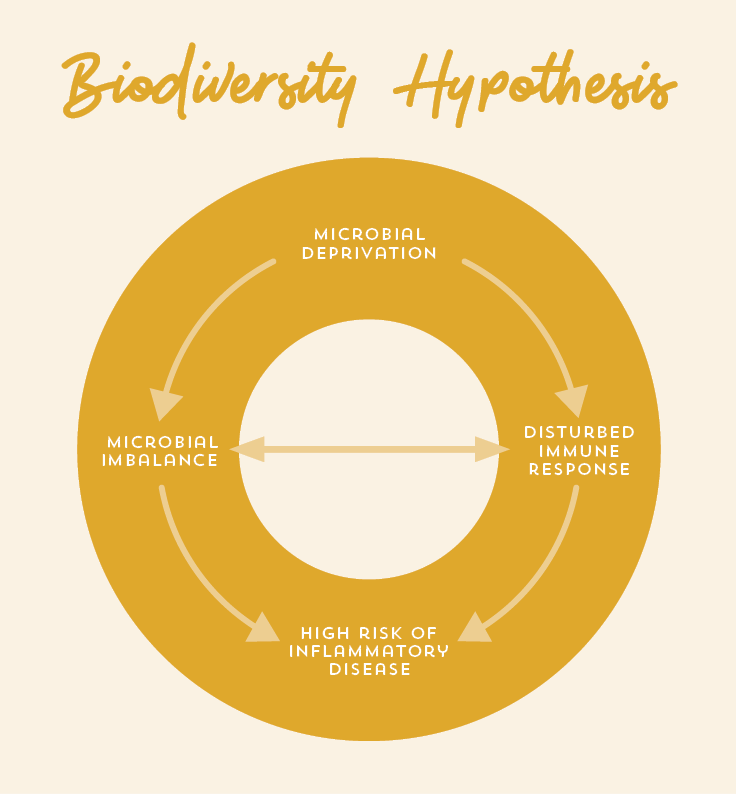
The hygiene hypothesis, a theory stating that a decline in childhood illnesses due to increased hygiene correlates over-cleanliness with the risk of developing allergic and inflammatory conditions, is getting attention as people become more concerned with hyper-vigilant germ-avoidance and dependence on antibacterial-everything in the shadow of Covid-19. This theory also places humans in the position of being the only organism experiencing an impact in this dynamic. Updated concepts, including the “old friends theory” or the “biodiversity hypothesis,” consider the relationship between humans and the environment to be reciprocal in nature: that humans are part of an interdependent web of existence, and our impact on microbes is just as important as theirs is on us.
We have been taught to think of all microorganisms—bacteria, viruses, parasites, and fungi—as dangerous things that must be avoided or eliminated. However, these small creatures are present—and are meant to be so—both inside and outside of the body, and play a critical role in digestion, skin health, immune function, and overall wellbeing. When humans were evolving in a context of hunting, gathering, and migration, our systems (and our DNA) learned to not only tolerate, but came to rely on the microorganisms in, on, and around them. Interaction with microbes, in fact, provided the opportunity for an immune system to become more resilient. As our species made revolutionary cultural shifts into agriculture, industry, germ theory, and the modern Anthropocene era (in which human activity has the greatest influence on Earth’s geology and ecosystems), our relationships with the natural world also shifted. Our dependence on our microbial “friends,” however, did not diminish. Even though many of us no longer drink from fresh lakes or wrangle with wild boars, our ancient DNA still expects to interact with a diverse array of microbes. Being denied contact with these organisms is just as harmful to our health as being deficient in nutrients like vitamin C.
We still interact with and acquire helpful organisms from the world around us from the moment (and method) of birth onward. Whether we are born vaginally or via c-section, whether we are breastfed or formula-fed, how many members are in our household, whether we interact with pets, or have a history of antibiotic use, these all play integral roles in our potential to encounter helpful organisms that will better prepare our bodies to fight off infection, parasites, and bacteria.
Germ Killers: Friend or Foe?
Over the past few generations, the use of antibiotics has increased exponentially. This includes not only their legitimate medical use to treat harmful infections, but also their ubiquitousness in such things as animal feed that can end up both on our plate and in our water supply, household products—like surface and hand sanitizers, toothpaste, hand soaps—and even in some children’s toys which contain antibiotics to keep them “sanitary.”
Because of antibacterial agents’ and broad-spectrum antibiotics’ ability to kill indiscriminately, both good and bad bacteria are on their radar. Antimicrobial products compromise our symbiotic relationship with microbes by denying our immune systems the exposure to helpful organisms they need. Additionally, this has the unintentional side effect of creating an environment for remaining organisms to adapt in order to survive the next onslaught. Antibiotics have been used so excessively that certain strains of bacteria have evolved to become resistant to our efforts to kill them, increasing the risk of potentially deadly and untreatable infections. The World Health Organization has identified antibiotic resistance as one of the greatest threats to global health—arguably more worrisome than the current pandemic.
Parents’ concern over the cleanliness of things their child touches existed well before Covid-19. Questions of “How clean is too clean?”, apprehension about over-protecting children from illness, and the immune system impact of antibacterial products have long been debated. It is increasingly shown that children with lower exposure to organisms than their bodies expect do not develop optimal immune function and are at a greater risk of infection, allergies, asthma, and other autoimmune and inflammatory diseases such as diabetes and inflammatory bowel disease. A clever study out of Sweden showed that children living in households where dishes were washed by hand (not sanitized) versus those washed in a dishwasher (sanitized) had a lower risk of developing allergic disease. The same researchers also showed that when parents cleaned a pacifier that had fallen on the floor with their own mouth, their children had a lower risk of allergies than did those whose parents ran that pacifier through the dishwasher.
Now excessive sanitization of hands and surfaces is being further compounded by mask-wearing, reducing the likelihood of transmitting airborne and respiratory droplets that contain viruses we might want young immune systems to build familiarity with, and reduced physical contact with others, leaving parents baffled at how to balance safety from Covid-19 with the need for developing and maintaining a healthy immune system.
Microbiome on your mind
A healthy microbiome, the array of helpful organisms in and on a person’s body, isn’t just good for physical health: it’s also critical to the development of good mental health (and vice versa!). Covid-19 hasn’t just compromised our microbiome health through overly-enthusiastic sanitization (since good old soap and water at relevant moments is all that is called for—see below), but the tremendous anxiety, fear of the unknown (including contagion), and the isolation that have resulted all play roles in suppressing immune function.
Social interaction with full facial exposure and physical contact in childhood is of critical importance to the development of good mental health, empathy, emotional regulation, problem solving, conflict resolution, and language, not to mention the benefits of acquiring those organisms necessary for building a healthy microbiome! Focusing on addressing the Covid-19 pandemic from a purely microbial perspective risks compromising one aspect of public health for another. Children do not appear to suffer significantly from infection with COVID-19, although they may play a role in spreading to others. Since it seems that the impact of this pandemic on health varies dramatically between age groups, it may be prudent to modify restrictions for different populations in order to mitigate the relative harms (e.g. allowing otherwise healthy children to interact freely among one another, while keeping them socially distant from the elderly or those with other health conditions).
Microbiome Maintenance During a Pandemic
While we have a collective responsibility to protect both the vulnerable and our public health resources, we also have a responsibility to protect our children’s larger health picture—immunologically, mentally, and socially. The measures currently being promoted do mean children are less likely to interact with the harmful virus that causes Covid-19, but also with the abundance of microbes that have the potential to be extremely beneficial to their health. How do we find a balance between the two so that one public health crisis is not exacerbated by our response to another?
While we exercise the public health recommendations during the pandemic, we can still allow for opportunities to get dirty! “Dirt-in-the-mouth” behaviour is a normal part of childhood and is arguably essential for optimal immune system development. Spending time playing outdoors and in nature, interacting with different people and animals within our social bubbles, eating a variety of foods, and touching as many things as possible (within reason!) will increase a child’s interaction with organisms that will help them build robust tolerance.
Even interactions with some potentially harmful germs (in the context of an otherwise healthy child who has the benefit of helpful microbes already in their system) provide opportunities for the immune system to learn how to respond effectively. It’s normal for children to get a common viral infection every month in their earlier years. As their immune systems learn how to discern between different infectious agents, their response becomes more efficient, resulting in fewer and less severe manifestations of coughs and colds. In fact, their bodies may have already dealt with them before symptoms get a chance to produce external evidence!
Clean Hands Club
Simple handwashing is basic hygiene practice that has had a huge impact on the risk of serious infectious disease. Children should continue to be reminded to wash their hands throughout the day before eating and after toileting, playing with animals, or sneezing, coughing, or blowing their nose. There is no need to use an antimicrobial agent: soap and water does the job just as well. The same strategies apply to household surfaces: wipe down high-contact surfaces regularly with a clean cloth and nothing more than baking soda or vinegar and water.
Go Wild Outside
Deliberately increase your child’s exposure to potentially helpful organisms. Walking outdoors in bare feet and getting hands in the dirt (think mud pies, gardening, and adventuring in the forest) have been shown to increase the array of helpful organisms on our skin and even inside the body. Interacting outside is also less conducive to the spread of the virus that causes Covid-19, and increases the opportunity for social interaction, physical activity, vitamin D production, unstructured play, and the myriad of other benefits alongside mental and emotional wellbeing that come from engaging in a natural environment.

Favour Fermented Flavours
Different parts of the body contain different types of bacteria, with over 10,000 different strains existing in the human microbiome. Eating a diet abundant in whole fermented foods can provide a natural source of beneficial bacteria. This is another beautiful example of how and why humans evolved to rely on microorganisms: in the years before refrigeration we relied on fermentation as a preservation strategy, utilizing our small friends to keep food available year-round. We became reliant on these organisms internally as well. Making homemade kombucha, yogurt, pickles, and sauerkraut is a fun family science experiment! The bacteria that reside in the digestive system are healthier, more diverse, and more useful to us when they are fed abundant prebiotic fibre (which probiotics feed on) in the form of a diet rich in fruits, vegetables, legumes, and whole grains.

Antibiotic Awareness
Avoid antibiotics in food and opt for organic and antibiotic-free, particularly in animal products. Stay away from household products that contain ingredients like triclosan or anything labelled as disinfectant. Question the necessity of any antibiotic prescription as many studies show that antibiotics are overprescribed, particularly for children.
Any household products stating antimicrobial or antibiotic properties are best to be avoided altogether. While antibiotic ingredients are useful in settings such as hospitals and doctor’s offices where its properties are specific to ensure our safety, widespread use can diminish their effectiveness over time, contribute to antibiotic resistance, and have negative environmental impacts, specifically through contaminated water run-off.
The following list of ingredients should be used sparingly and avoided if possible.
- Alkyl dimethyl benzyl ammonium chloride
- Cloflucarban
- Fluorosalan
- Hexachlorophene
- Tribromsalan
- Triclocarban
- Triclosan
Healing after antibiotics
Sometimes antibiotics are necessary. Since antibiotics will wipe out both beneficial and infectious microbes, restoring the microbiome after a course of antibiotics will help support the maintenance of optimal health and healing. Increase your intake of microbiome-friendly foods and/or include supplemental probiotics that provide a variety of microorganisms. Talk to your healthcare provider to find out which strain and how much is right for your specific needs.

Befriend the Microbiome
Rather than becoming embroiled in the narrative of fear and anxiety about the agents that cause Covid-19, influenza, and ear infections, nurture an acceptance of (and dare we say, a gratitude for!) the microbes that are all around and in us, explaining how some help while some are not so friendly. By teaching our children to care for themselves in other ways, like eating and sleeping well, getting enough exercise and time outdoors, and managing stress, they will have the foundations for a healthy and reciprocal relationship with their microbial friends.
Microorganisms are present everywhere and we underestimate both how important they are to our physical, mental, and emotional wellbeing, as well as the great (and misguided) effect we have had on them. Covid-19 has drastically changed how we conduct our daily lives, especially when it comes to cleanliness and personal interaction. Our heightened awareness, diligent sanitization, social distancing and the way we discuss them will be communicated to our children. If, in our enthusiasm to protect them from exposure, we wipe away all the microbial “good guys” with the bad, we may inadvertently do more harm than good. While, indeed, your priority during this pandemic is to protect yourself and your family, don’t forget about the little “friends” that are working hard to protect you too!
You may also enjoy: Exploring the Mysterious Microbiome, How Vitamin D and Probiotics Support Your Child's Immunity, and Healthy Skin Comes from the Gut.






